Customizing Implants With 3D Image Processing
Long-term patient comfort is a key part in any implant surgeries. Accurate placements of implants, of knees, hips, and other medical devices, is crucial to reducing the risk of discomfort and the need for costly revision surgeries. Custom-designed implants and simulation is a field of growing importance, giving clinicians and designers freedom to tailor designs for patients and make more informed surgical decisions. In addition to streamlining the manufacturing process, this approach enables multiple implant variations and pathologies to be considered at the virtual stage through additive manufacturing. This is as opposed to finding and correcting problems through trial and error.

3D image processing of patientspecific implants with Synopsys Simpleware Software.
The potential of custom and simulation-based presurgical planning crosses into many significant trends: topology optimization, finite element analysis (FEA), composites/materials testing, reverse engineering, 3D printing, and regulatory compliance. Several companies are using 3D image-based modeling to design and test the performance of implants, in a noninvasive way.
Work carried out by Corin Group, 360 Knee Systems, and other businesses demonstrate successful and repeatable workflows for linking 3D scans of patients with software tools like Synopsys Simpleware™, 3D printing, and laser-guided surgeries. The following case studies outline steps used to solve challenges in implant design with image-based methods, while aiming to highlight some of the key questions associated with developing and using this technology.
![]() Key Opportunities in Personalized Implants
Key Opportunities in Personalized Implants
Medical image data, such as computed tomography (CT) or magnetic resonance imaging (MRI), captures realistic geometries of patients from scans. Using these patient-specific anatomy, procedures and implant designs can be tailored to individual needs and pathologies. Rather than taking a generalized approach to medical device design, researchers and clinicians do take into account variation. In addition, scans of failed implants can help to better understand why some devices fail and what steps — in the surgical planning process — can be altered to reduce the risk of recurrence.
 An anatomical model generated from image data using Synopsys Simpleware software.
An anatomical model generated from image data using Synopsys Simpleware software.
There is worldwide demand for customizing orthopedic solutions and for increasing the use of computer simulation to reduce the risk of errors. One method that is increasingly being explored by medical device manufacturers and regulatory bodies such as the FDA is computational simulation using FE models created from biomedical imaging. These models break down complex anatomies into numerical representations that allow realistic analysis to be carried out of different scenarios.

A polyethylene tibial insert (left) and an accurate 3D model generation from micro-CT data using Synopsys Simpleware ScanIP (right). (Credit: Prof. Alister Hart, MD, University College London and the Royal National Orthopaedic Hospital)
FDA is recognizing this method as part of the validation of medical devices by manufacturers, reducing the burden of more traditional physical testing. Virtual testing of the implant’s performance is included when it is created using additive manufacturing processes; this enables a better understanding of as-manufactured performance before it is placed inside a human body. Simulation using realistic models provides surgeons with more information when planning operations. Manufacturers are provided with increased data when testing prototypes and checking for potential errors.
![]() Key Challenges for 3D Medical Image Model Generation
Key Challenges for 3D Medical Image Model Generation
However, despite its promise, challenges still remain for customizing implants through image-based simulation. These include the potentially time-consuming process of working with 3D medical images to identify regions of interest and to prepare the highest-quality models for simulation. The workflow of going from a scan to a 3D computational or FE model can be interrupted by problems with ensuring the quality of exported models, including for additive manufacturing.
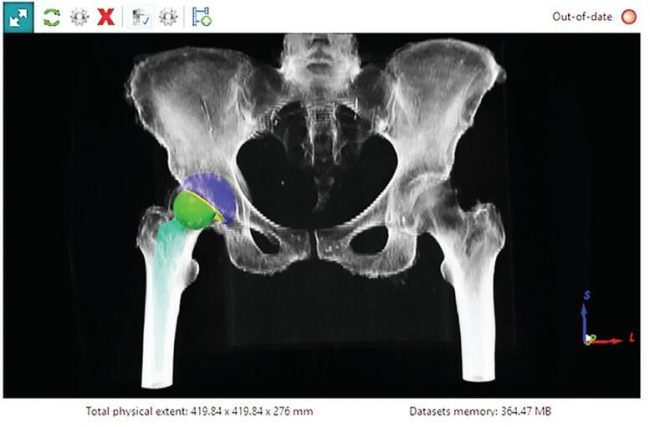
A hip model generated using Synopsys Simpleware software for Corin Group.
In addition, creating design iterations from scan data often requires repetitive work to test out multiple variations on an implant prototype. Efficient workflows that align with preclinical planning protocols require confidence in model accuracy. Several medical device manufacturers and researchers are finding solutions to these challenges through workflows that streamline image-based techniques through specific software methods.
 360 Knee Systems examine implant placement in the knee.
360 Knee Systems examine implant placement in the knee.
![]() Creating Better Patient-Specific Models
Creating Better Patient-Specific Models
Solutions focus on linking different stages of scanning, processing of resulting image data, and exporting to simulation and additive manufacturing. Orthopedic manufacturers such as Corin Group have achieved particular success at establishing robust, repeatable workflows for medical device designs. The Australia-based Corin Group’s Optimized Positioning System (OPS) technology uses Synopsys Simpleware software tools to help surgeons plan total hip replacement (THA) operations.
THA procedures typically rely on literature-derived “safe zones” to define the best placement of acetabu-lar components. However, this approximation cannot account for patient variety, with clinical research showing that up to 50 percent of hip surgeries miss their target orientation.1 For patients, this means problems with comfort and risks of dislocation and revision surgeries. Corin Group therefore applies patient-specific simulation technology to improve accuracy and reduce these risks.
Corin Group’s OPS system uses 3D scans of patient anatomies, taken from computed tomography (CT) and x-ray tomography. The data is imported to Synopsys Simpleware software and processed by engineers to segment regions of interest for hip placement. At this stage, landmarks are placed on the skeleton for implant placement. These steps can be time-intensive, but have been sped up through Simpleware software’s semi-automated segmentation tools, as well as through scripting tools that generate repeatable results.
Once a patient-specific model is generated, the OPS system is used to analyze different types of movement and orientation within routine physiological activities. This testing aims to identify the optimal position of the acetabular cup during pelvic rotations. Simpleware software allows Corin engineers to import computer-aided design (CAD) implants to a patient’s data and produce 3D printed surgical guides that can be used by surgeons to improve the chance of positive intraoperative results. Virtual testing of implant position is valuable for reducing a reliance on physical experimentation and the literature to achieve optimal results. During surgeries, the 3D printed guides are combined with laser-guided alignment system to assist positioning.

Custom-designed implants reduce the risk of discomfort and the need for revision surgery. 3D images of patients makes it easier to reduce the risk of poor fitting implants.
Similar approaches are being developed by companies such as the 360 Knee Group, which uses 3D scans to create knee models in Simpleware software for studying optimal implant positions. As with hip replacements, being able to link 3D images of patients with virtual planning and presurgical guides makes it easier to reduce the risk of poor fitting and improve the accuracy and reliability of implants.2
Other applications for image-based modeling are being tested by Dr. Harry Hothi at University College London (UCL) to tackle the problem of knee revision surgeries.3 Suboptimal orientation of femoral and tibial components can lead to long-term patient issues, including pain and wear. Research at UCL studies retrieval and clinical data from CT to evaluate materials damage. Simpleware software was used to segment the data and to create a surface model suitable for comparing pre-revision implant positioning with post-revision micro-CT scans of failing inserts. This method enables a better understanding of the correlation between implant orientation and wear pattern, potentially reducing future problems with patient-specific designs.
Surgeons use the UCL research to improve understanding of which implant design is best suited for particular problems, for example size mismatches, and whether a surgery is necessary depending on the likelihood of future problems. The more data available to surgeons and other clinicians, the easier it becomes to make decisions that carry significant financial costs and potential issues for patients.
The potential of image-based modeling for customizing implants can be seen in recent work by Rob Stupplebeen in the treatment of arthritis. Stupple-been used Simpleware software to rapidly process CT data of the hand before integrating models with prosthetics and simulating strain in Abaqus/CAE software. The workflow demonstrated how a CAD and image-based method provides virtual planning insights for clinicians looking to optimize implants from individual patient scans.
![]() Conclusions
Conclusions
The scope of using image-based modeling for customizing implants and other surgical techniques is broad.
Researchers in fields as diverse as design of neuromodulation devices and wheelchairs are able to use accurate 3D models of body parts and planned CAD models of devices to evaluate fit and conditions for varying patients and users.4,5 The gradual recognition of simulation as a validation tool by the FDA and other organizations is creating demand for faster and more accurate methods that remain reliable for clinicians.
Challenges to the growth of this method include the availability of clinical scan data, and the learning curve for radiologists and other users to learn image processing and model-generation techniques. In addition, software solutions require both the ability to carry out tasks to meet the tight deadlines typically required for surgeries, as well as to make workflows intuitive and repeatable at sufficient scale to deliver usable results.
However, with the uptake of image processing tools like Simpleware software and regulatory validation, clinical researchers and those involved in presurgical planning have access to robust and benchmarked methods. Together with the growth of additive manufacturing as a way of optimizing the design of patient-specific implant, there is strong potential for creating more tailored devices that take different pathologies into consideration.
Source: medicaldesignbriefs



Recent Comments